Abstract
INTRODUCTION
Extreme neutrophilic-predominant leukocytosis is frequently alarming to clinicians and often triggers expedited evaluation to distinguish between myeloid malignancies (MM), such as chronic myeloid leukemia (CML), and non-malignant etiologies. The term "leukemoid reaction" has been used to describe the latter case - episodes in which a patient's white blood cell (WBC) count is greater than 50k/μL from causes other than leukemia. MM account for only a minority of neutrophilic leukocytosis, but diagnostic testing for these entities involves expensive and time-consuming sequencing tests. Therefore, it would be valuable to identify factors that are routinely and rapidly available and that can distinguish between these identities to prioritize work-ups and allow for more judicious use of molecular testing. Prior studies attempting to address this problem have been limited to small case series or have focused on a single diagnosis. We sought to identify such factors using a large data set with modern testing modalities.
METHODS
Adult patients > 18 years of age with extreme neutrophilic leukocytosis from 2000-2020 at a tertiary care hospital were included. Extreme neutrophilic leukocytosis was defined as a leukocyte count greater than 50k/μL on at least 1 occasion, with granulocytes accounting for more than 50% of leukocytes. Patients were excluded if the cause of their leukocytosis was iatrogenic (e.g., G-CSF). Researchers performed individual chart review to determine the cause of a patient's leukocytosis, grouping each into one of four categories: (i) leukemoid reactions (LR); (ii) MM; (iii) non-myeloid malignancies; and (iv) mixed leukemoid and malignant etiologies (e.g., a leukemoid reaction in a patient with an underlying myeloproliferative neoplasm). The following patient characteristics were analyzed at the time of first presentation with WBC > 50k/μL: age, hemoglobin, MCV, platelet count, differential, LDH, uric acid, ferritin, and CRP.
RESULTS
We identified 214 patients who fit our inclusion criteria: MM accounted for 67/214 (31%) cases, while 101/214 (47%) described LRs. Non-myeloid neoplasms accounted for 19/214 patients and 27/214 had mixed etiologies.
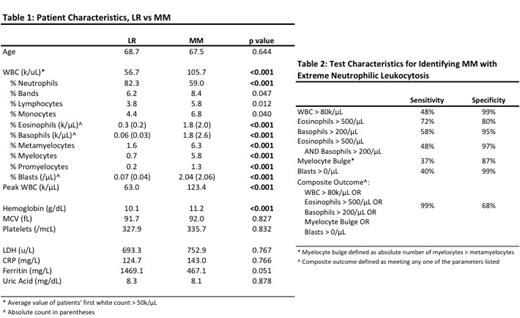
Our primary aim was to identify factors that distinguish between MM and LR. Mean age at presentation did not differ (68.7 vs. 67.5, p=0.64), though 6-month mortality was much higher in those diagnosed with LR vs MM (63.3% vs. 13.4%, p<0.01). When patients with MM were discovered to have extreme leukocytosis, they tended to have higher white counts on initial presentation (105.7 vs 56.7, p<0.01) and higher peak white counts during a given hospitalization (123.4 vs 63.0, p<0.01). White counts >80k/μL on presentation were 99% specific (with sensitivity 48%) in identifying MM.
Analysis of the differentials revealed that LR were more neutrophil predominant (83% vs. 59%, p<0.01) and that "significant neutrophilia" (defined as neutrophilia >90%) was 97% specific (27% sensitive) in distinguishing LR from MM. Mild eosinophilia (absolute eosinophils >500/μL) and basophilia (absolute basophils >200/μL) were 72% and 58% sensitive and 80% and 95% specific, respectively, for MM.
The discriminative power of a myelocyte bulge was also analyzed. MM tended to have more metamyelocytes (6.3% vs. 1.6%, p<0.01) and myelocytes (5.8% vs 0.7%, p<0.01), though a true "myelocyte bulge" (absolute myelocytes > metamyelocytes) was only 37% sensitive and 87% specific in distinguishing between MM and LR.
Lastly, meeting any one of the parameters in our composite outcome (Table 2) proved 99% sensitive and 68% specific for MM.
CONCLUSIONS
In our retrospective analysis of extreme neutrophilic leukocytosis, the most common cause was leukemoid reactions, which were associated with far greater mortality than malignant etiologies. Patients with MM had higher admission and peak white counts. They also tended to present with eosinophilia and basophilia, and though neither universally defined MM, the combination of these parameters was specific for distinguishing between our groups. The presence of blasts, too, was specific for MM, though notably, were also seen in rare LRs. Finally, the sensitivity of our composite outcome suggests that patients who meet none of those criteria may be able to avoid unnecessary workups for MM. Notable negative results included findings that platelets, CRP, and LDH were not useful in discriminating between LR and MM.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal